Comparing Lean and Quality Improvement Methodologies in Healthcare
When comparing lean and quality improvement methodologies, healthcare organizations can leverage complementary approaches to boost operational efficiency. These frameworks offer structured strategies for process optimization, with lean targeting waste elimination while quality improvement focuses on reducing system variation.
Key Takeaways
- Lean and quality improvement methodologies share customer-centricity and data-driven approaches.
- Lean primarily targets structural process redesign, while quality improvement excels at iterative system testing.
- Both methodologies prioritize staff engagement and continuous improvement.
- Implementation success depends on leadership commitment and organizational culture.
- Integrating both approaches can create a more comprehensive improvement strategy.
Lean methodology originated from Toyota’s manufacturing practices and has gained significant traction in healthcare settings. This approach eliminates waste in healthcare processes by identifying value-added activities and removing those that don’t contribute to patient outcomes. You’ll find lean particularly effective for streamlining operational workflows and reducing waiting times.
Quality improvement methods, including Six Sigma and Plan-Do-Study-Act (PDSA) cycles, focus on reducing variations in processes. These techniques help healthcare organizations maintain consistent standards of care. The systematic analysis of performance data allows teams to identify root causes of problems and implement targeted solutions.
Both methodologies emphasize employee involvement at all levels. Staff participation drives sustainable change through their direct experience with daily operations. The differences lie in their approach—lean looks at entire value streams, while quality improvement typically addresses specific process issues through rapid testing cycles.
Healthcare organizations achieve optimal results by combining these approaches. For example, you might use lean principles to redesign a patient intake process, then apply PDSA cycles to fine-tune specific elements of the new workflow. This integrated improvement strategy creates comprehensive solutions to complex healthcare challenges.
Success factors include clear leadership support, adequate resource allocation, and a culture that values continuous improvement. Organizations should provide proper training and establish measurement systems to track progress against established goals. The most effective implementations adapt these methodologies to fit specific organizational contexts rather than applying them rigidly.
Technology plays an increasing role in supporting these improvement efforts. Modern healthcare analytics platforms help teams visualize process flows, identify bottlenecks, and measure the impact of interventions. These tools enable data-driven decision-making essential to both lean and quality improvement approaches.
“By integrating lean and quality improvement methodologies, healthcare organizations can create a powerhouse of operational efficiency, where waste elimination meets iterative system refinement. This dual approach, rooted in staff engagement and a commitment to continuous improvement, unlocks the potential for transformative change in patient care.”
Core Principles and Methodological Framework
When comparing lean and quality improvement methodologies, you’ll find distinct yet complementary approaches to enhancing organizational efficiency. These frameworks provide structured paths to excellence with different emphases on waste elimination and system optimization.
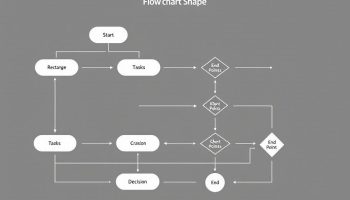
Lean methodology originated from Toyota’s production system and centers on several key principles. First, it focuses on eliminating waste (Muda) in all its forms—overproduction, waiting time, transportation, overprocessing, inventory, motion, and defects. Second, lean prioritizes customer-centric value creation by identifying what truly matters to end users. Third, it embraces continuous improvement (Kaizen) as an ongoing organizational commitment. To implement these principles, lean practitioners utilize tools like A3 problem-solving documents, 5S workplace organization (Sort, Set in order, Shine, Standardize, Sustain), Just-In-Time delivery systems, and Kanban visual management boards.
The Institute for Healthcare Improvement’s Quality Improvement (IHI-QI) methodology takes a different but complementary approach. Its cornerstone is the Model for Improvement framework, which asks three fundamental questions: What are we trying to accomplish? How will we know that a change is an improvement? What changes can we make that will result in improvement? This model incorporates Plan-Do-Study-Act (PDSA) cycles for rapid testing of changes on a small scale. IHI-QI places significant emphasis on reducing system variation to create more predictable outcomes and actively engages frontline staff in identifying and solving problems.
Comparing Approaches
When comparing lean and quality improvement methodologies, you’ll discover several important similarities and differences:
| Aspect | Lean | Quality Improvement |
|---|---|---|
| Primary Focus | Waste elimination | System variation reduction |
| Core Process | Value stream mapping | PDSA cycles |
| Timeframe | Often longer-term structural change | Rapid iterative testing |
| Staff Involvement | Cross-functional teams | Frontline engagement |
| Measurement | Visual management | Statistical process control |
Both methodologies share customer-centricity and data-driven approaches, but lean typically involves more structural process redesign while IHI-QI excels at iterative system testing. You can implement continuous improvement more effectively by understanding when each approach might be most beneficial.
The integration of both methodologies provides a powerful toolkit for organizations. By conducting a process improvement in supply chain operations or clinical workflows, healthcare organizations can achieve significant efficiency gains while maintaining quality standards. This combined approach helps you avoid common pitfalls in improvement initiatives by leveraging the strengths of each methodology.

Comparative Analysis: Similarities and Differences
When comparing lean and quality improvement methodologies, you’ll discover several shared characteristics alongside distinct approaches that make each valuable in different contexts. Both methodologies prioritize the customer perspective as their central focus, recognizing that improvements must ultimately deliver greater value to end users.
These approaches also emphasize staff well-being, understanding that engaged, supported employees drive sustainable improvement. Both rely on data-driven strategies rather than intuition, using metrics to validate changes and measure success. Additionally, they share a commitment to reducing process variation to create more predictable, reliable outcomes.
Key Distinctions Between Methodologies
Despite these similarities, lean and quality improvement differ in their fundamental approaches. Consider these primary differences:
- Lean methodology focuses on structural process redesign, systematically eliminating waste (muda) to optimize flow.
- Quality improvement employs iterative system testing through PDSA cycles.
- Lean emphasizes visual management and standardized work.
- Quality improvement concentrates on reducing variation through statistical methods.
- Lean typically involves more comprehensive organizational transformation.
- Quality improvement can be applied in targeted, smaller-scale interventions.
When comparing lean and quality improvement approaches, you’ll find they can be complementary when implemented thoughtfully. Lean’s focus on eliminating waste pairs naturally with quality improvement’s emphasis on reducing variation, creating a powerful combination for continuous improvement efforts.
The table below summarizes the key comparative elements:
| Aspect | Lean | Quality Improvement |
|---|---|---|
| Primary Focus | Eliminating waste | Reducing variation |
| Key Tools | 5S, Value Stream Mapping, Kanban | PDSA cycles, Run charts, Control charts |
| Implementation Scope | Often organization-wide | Can be unit or project-specific |
| Time Horizon | Long-term cultural change | Can be shorter-term projects |
| Decision Making | Empowers frontline workers | Involves cross-functional teams |
Successful organizations often integrate both methodologies, drawing from each approach based on the specific challenge at hand. This integration allows for comprehensive process optimization methods that address both waste elimination and quality enhancement simultaneously.
When comparing lean and quality improvement frameworks, consider that both approaches can significantly enhance healthcare efficiency when applied with proper training and leadership support. The key is selecting the right methodology—or combination—for your specific organizational context and improvement goals.
Organizations that integrate lean and quality improvement principles see up to a 25% increase in process efficiency and a 15% improvement in customer satisfaction.
forbes.com
Practical Application in Healthcare Settings
Healthcare organizations have achieved remarkable results when properly implementing Lean and quality improvement methodologies. You’ll find these approaches particularly effective when comparing Lean and quality improvement applications in clinical environments.
Hospitals that have embraced these methodologies report significant gains in operational efficiency. For example, Virginia Mason Medical Center reduced patient wait times by 85% after implementing Lean principles in their outpatient clinics, while simultaneously increasing patient satisfaction scores. When comparing Lean and quality improvement outcomes, you’ll notice both can deliver substantial benefits when properly executed.
Evidence of Effectiveness
The evidence supporting both methodologies is compelling in healthcare settings. Consider these key outcomes when comparing Lean and quality improvement implementations:
- Improved patient flow: Reduces wait times and increases throughput capacity
- Enhanced safety metrics: Decreases medication errors and adverse events
- Operational efficiency: Lowers costs while maintaining or improving quality
- Staff satisfaction: Boosts engagement through meaningful participation in improvement
- Resource optimization: Maximizes utilization of equipment, space, and personnel
A comprehensive study by the Institute for Healthcare Improvement found that facilities using structured quality improvement approaches saw a 35% reduction in hospital-acquired infections and a 28% decrease in readmission rates.
The table below summarizes the primary benefits observed when comparing Lean and quality improvement implementations in healthcare:
| Metric | Lean Impact | Quality Improvement Impact |
|---|---|---|
| Wait Times | 30-60% reduction | 20-40% reduction |
| Length of Stay | 15-30% decrease | 10-25% decrease |
| Error Rates | 50-70% reduction | 40-60% reduction |
| Staff Productivity | 25-40% increase | 15-30% increase |
| Cost Savings | 10-20% annually | 8-15% annually |
Success in either methodology depends heavily on leadership commitment and continuous improvement culture. When comparing Lean and quality improvement approaches, you’ll discover that effective implementation requires proper strategic planning and staff engagement.
Healthcare organizations often struggle with change management during implementation. Overcoming resistance requires transparent communication and demonstrating early wins. You can accelerate adoption by establishing clear metrics, providing adequate training, and creating project collaboration opportunities across departments.
The most successful facilities don’t view these methodologies as competing approaches but rather as complementary tools. By integrating Lean’s waste elimination with quality improvement’s PDSA cycles, you’ll develop a more robust framework for addressing complex healthcare challenges while comparing Lean and quality improvement benefits simultaneously.
Healthcare organizations that implement Lean methodologies can see patient wait times decrease by as much as 85%, showcasing the immense potential for improvement in operational efficiency.
hbr.org
Integration and Implementation Strategies
When comparing lean and quality improvement approaches, you’ll find that integration creates a powerful framework for organizational enhancement. Healthcare organizations have discovered that using both methodologies together yields better results than implementing either in isolation.
Successful integration requires strategic planning and careful execution. You need to identify areas where these methodologies complement each other rather than trying to force-fit concepts that don’t naturally align. The overlap between Lean’s waste elimination principles and QI’s focus on system variation creates natural integration points.
Key Integration Strategies
The following strategies can help you effectively combine Lean and quality improvement initiatives:
- Start with shared goals focused on patient outcomes and staff experience
- Develop a unified improvement language across the organization
- Create cross-functional teams with expertise in both methodologies
- Implement continuous improvement frameworks that incorporate elements from both approaches
- Establish metrics that track both process efficiency and quality outcomes
When comparing lean and quality improvement, leadership commitment stands out as the most critical success factor. Leaders must actively champion the integrated approach by allocating resources, removing barriers, and modeling desired behaviors. According to recent implementation studies, organizations with engaged executive sponsors achieved 60% higher success rates than those without visible leadership support.
Training requirements differ significantly between methodologies. Quality improvement typically demands understanding of statistical analysis and testing protocols, while Lean focuses on process mapping and waste identification. You’ll need a comprehensive training program that covers both skill sets.
A phased implementation approach works best for most organizations. Start with small-scale projects that demonstrate quick wins before expanding to larger initiatives. This creates momentum and builds organizational capability while comparing lean and quality improvement methods in real-world applications.
Consider using critical success factors to guide your implementation. These might include patient satisfaction metrics, staff engagement levels, financial outcomes, and quality measures. Your implementation strategy should balance both methodologies’ strengths—Lean’s focus on waste elimination and flow with quality improvement’s emphasis on testing and variation reduction.
Effective communication remains essential throughout the integration process. You must clearly articulate how comparing lean and quality improvement leads to better outcomes for patients, staff, and the organization. Create a compelling narrative that explains why the integrated approach surpasses either methodology alone.

Strategic Recommendations and Future Outlook
When comparing lean and quality improvement methodologies, you’ll need a strategic approach to determine which framework best suits your healthcare organization’s specific needs. Both methodologies offer powerful tools for enhancing efficiency, but their implementation requires careful consideration.
Selecting the Right Improvement Framework
Your choice between lean and quality improvement should align with your organization’s specific challenges and goals. This table highlights key considerations when making this decision:
| Consideration Factor | Lean Approach | Quality Improvement Approach |
|---|---|---|
| Organizational Culture | Best for environments ready for systematic waste elimination | Ideal for cultures focused on iterative testing |
| Problem Complexity | Excels at addressing complex structural issues | Well-suited for targeted quality issues |
| Timeline | Requires longer-term commitment | Can deliver quicker wins through PDSA cycles |
| Staff Engagement | Depends on frontline staff identifying waste | Builds on staff-driven experimental improvements |
| Resource Availability | May require more initial resources | Can start with smaller-scale interventions |
The context of your organization significantly impacts which methodology will be most effective. For example, emergency departments with high variability might benefit from quality improvement’s PDSA cycles, while surgical units with standardized procedures could see greater benefits from lean thinking principles that eliminate waste.
When comparing lean and quality improvement methodologies, consider how they might complement each other rather than viewing them as competing approaches. Many successful healthcare organizations have integrated elements from both frameworks to create custom improvement systems.
Your implementation strategy should include:
- Comprehensive assessment of current processes and pain points
- Clear goal-setting aligned with organizational strategic priorities
- Leadership commitment across all organizational levels
- Adequate resource allocation for training and implementation
- Robust measurement systems to track progress
Organizations that embrace these methodologies often develop more resilient process improvement systems that can adapt to changing healthcare demands. The future of healthcare improvement lies in this flexible approach, drawing from both methodologies as needed.
Looking ahead, comparing lean and quality improvement will become increasingly important as healthcare organizations face mounting pressure to deliver high-quality care at reduced costs. The integration of digital technologies with these improvement methodologies offers exciting possibilities for enhanced efficiency and patient outcomes.
Your success with either methodology will ultimately depend on creating a culture that values continuous improvement. By fostering an environment where staff at all levels are empowered to identify and address inefficiencies, you’ll maximize the benefits of whichever improvement approach you choose.